내시경으로 진단 및 치료한 대장 평활근종
Colon Leiomyoma Diagnosed and Treated with Endoscopy
Article information
Trans Abstract
Leiomyoma is a benign smooth muscle tumor that may occur throughout the entire digestive tract. It occurs more frequently in the stomach and the small intestine, but is rarely seen in the large intestine. Here, we report two cases of colon leiomyoma mimicking the appearance of colon polyps that were found incidentally. They were simultaneously diagnosed and treated by endoscopic mucosal resection. Careful and thorough endoscopic examination is required for differential diagnosis of polyps that may actually be subepithelial tumors.
INTRODUCTION
Leiomyomas arising in the colon and rectum are uncommon, accounting for only about 3% of all gastrointestinal leiomyomas [1-5]. They are mostly found incidentally, but some large lesions may cause symptoms, such as abdominal pain, rectal bleeding, and perforation [1-5]. Due to the difficulty of distinction between benign and malignant tumors, the possibility of recurrence and insensitivity of these tumors to adjuvant therapies, surgical removal of tumors larger than 2 cm is recommended [1]. Here, we report two cases of colon leiomyoma that were diagnosed and treated by endoscopic mucosal resection.
CASE REPORT
Case 1
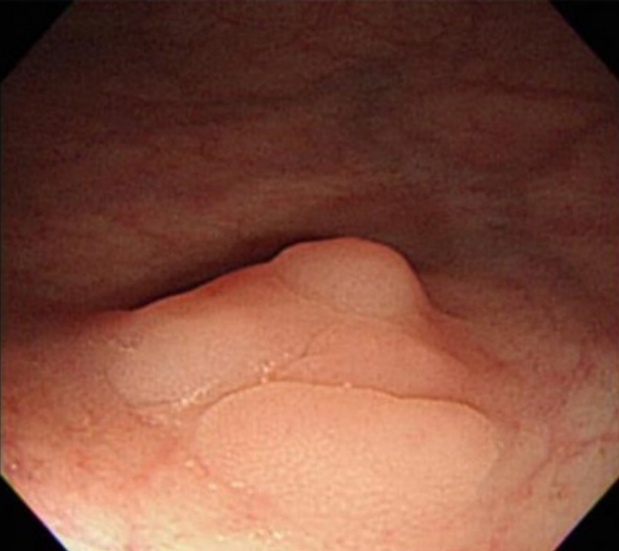
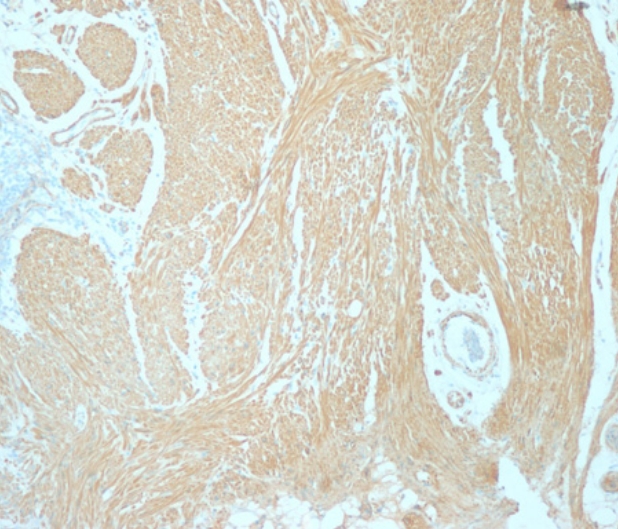
A 72-year-old woman came to the outpatient department for upper endoscopy, colonoscopy, and abdominal sonography due to indigestion. She was taking calcium channel blocker for hypertension with gastrointestinal motility drugs due to chronic indigestion. At age 67, she was diagnosed with breast cancer and underwent right mastectomy. At the endoscopy center, vital signs were stable. Blood tests showed no abnormal results. Abdominal sonography showed a hepatic cyst, a renal cyst, and bilateral renal parenchymal disease was suspected. Reflux esophagitis with chronic superficial gastritis was observed on upper endoscopy examination. Colonoscopy examination revealed several diverticula at the hepatic flexure and the sigmoid colon. A sessile nodular type polyp measuring about 0.8 cm with pale mucosa demarcated from the surrounding normal mucosa was noted on the distal rectum (Fig. 1). Injection with a mixture of carmine and saline was done to lift the lesion for polypectomy. The resected surface showed no remnant tissue from the polypoid lesion. To prevent bleeding after polypectomy, two endoclips (EZ Long, Olympus, Tokyo, Japan) were applied. The lesion was removed completely. Immunohistological findings were negative for cluster of differentiation (CD) 34 and CD117 but positive for caldesmon (Fig. 2). Leiomyoma arising from the muscularis mucosa was confirmed by pathology. No bleeding or perforation was noted after polypectomy.
Case 2
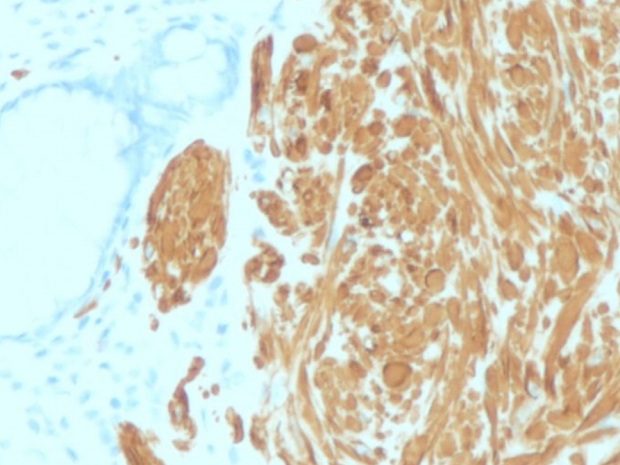
A 47-year-old man came to the health center for a general medical checkup. He did not have any gastrointestinal symptoms. Vital signs were stable. Laboratory examination showed no abnormal findings except elevated triglyceride and low-density lipoprotein cholesterol. Abdominal sonography revealed fatty liver. Chest X-ray and urine examination showed no abnormal findings. Upper endoscopy showed reflux esophagitis. Colonoscopy exam revealed a protruded type polyp measuring 8 mm (Fig. 3) and submucosal injection with polypectomy was done with snare (Boston Science). The surface of the polyp appeared pale with sharp demarcation from the surrounding normal mucosa. Leiomyoma was confirmed by pathology (positive for desmin and negative for c-kit) (Figs. 4 and 5). Leiomyoma arising from the muscularis mucosa was confirmed by pathology and it was removed completely grossly and pathologically.
DISCUSSION
Leiomyoma is a benign smooth muscle tumor, which can arise from the muscularis mucosa, muscularis propria, or vascular smooth muscle [1,2]. Most gastrointestinal leiomyomas occur in the stomach or the small intestine, while the large bowel accounts for only 3% of more cases, and they are detected more frequently in the sigmoid and transverse colon [3-5]. The majority of leiomyomas are sessile intraluminal or intramural tumors with a normal overlying mucosa. The peak incidence occurs in the third decade of life with a slight female predominance [2]. Colonic leiomyomas are usually asymptomatic and are detected incidentally during screening colonoscopy [5-8]. The clinical manifestations depend on the location, size, and direction of tumor growth. Large lesions can cause abdominal pain, intestinal obstruction, rectal bleeding, and perforation [2,4,7]. Surgery is the treatment of choice for large leiomyomas [9,10]. Small leiomyomas can appear as conventional polyps, which may alter the method used for removal. Careful and thorough endoscopic examination is required to differentiate polyps from subepithelial lesions.