 |
 |
| Korean J Med > Volume 100(3); 2025 > Article |
|
Abstract
Immunoglobulin G4-related disease (IgG4-RD) is a fibroinflammatory condition characterized by the tendency to form tumefactive lesions. However, the disease has highly variable clinical manifestations, as IgG4-RD can affect any organ. The biliary tree and major salivary glands are commonly affected; however, bowel mucosa is rarely affected. A 41-year-old man presented to our hospital complaining of abdominal pain. Computed tomography and endoscopy were performed at another hospital, and a biopsy was performed on a lesion suspected to be malignant. Biopsy revealed no remarkable findings other than lymphoid hyperplasia. Subsequently, IgG4-RD was confirmed via surgical biopsy. The disease and its symptoms were successfully treated with steroid therapy.
Immunoglobulin G4-related disease (IgG4-RD) is a fibroinflammatory condition characterized by a tendency to form tumefactive lesions. However, the disease has highly variable clinical manifestations and can affect any organ system. Commonly affected organs include the pancreas, biliary tree, major salivary glands, periorbital tissues, kidneys, lungs, lymph nodes, and retroperitoneum. Additionally, the involvement of the meninges, aorta, prostate, thyroid, pericardium, skin, and other organs in IgG4-RD has been well described. However, the disease rarely affects the brain parenchyma, joints, bone marrow, or bowel mucosa [1]. IgG4-RD involvement in the gastrointestinal tract appears to be rare and has only been reported as case reports to date, including patients with morphological changes, ulcer stricture, and submucosal tumors [2]. A few cases of IgG4-RD involving the bowel mucosa, mistaken for lymphoma and subepithelial tumors, have been reported [3,4].
Here, a biopsy was performed on a polypoid lesion in the gastrointestinal tract, identified through imaging and endoscopy, in a patient with persistent abdominal pain. Although endoscopic mucosal biopsy revealed no specific findings other than lymphoid hyperplasia, surgical biopsy confirmed IgG4-related disease. As primary IgG4-RD in the gastrointestinal tract is uncommon, we report this case along with a literature review.
A 41-year-old man visited the gastroenterology and hepatology department of our hospital complaining of abdominal pain. The patient had been experiencing intermittent throbbing pain in the right lower abdominal quadrant for 3 weeks, with a numerical rating scale score of 3. He visited a hospital close to his residence for an examination. However, the cause remained unclear, and his abdominal pain appeared to have worsened.
He had no significant medical history except for undergoing surgery in 2012 to treat an epidural hemorrhage in his brain, which was caused by a car accident. The patient drank alcohol twice a week (half a bottle of soju) and did not smoke. He worked at a recycling center. Regarding family history, his mother had been diagnosed with diabetes. Apart from abdominal pain, he had no gastrointestinal symptoms such as diarrhea, constipation, nausea, or vomiting. On physical examination, his abdomen was soft and flat, with normoactive bowel sounds. Abdominal tenderness was noted in the lower-right quadrant, but no rebound tenderness was observed. The results of the other examinations were unremarkable.
The patient underwent endoscopy at another hospital. A 2-cm protruding mass-like lesion in the duodenal bulb (Fig. 1) and non-contiguous polypoid lesions in the ascending and transverse colon were identified (Fig. 2), and a biopsy was performed. Biopsies of the duodenal and colon specimens revealed chronic inflammation or lymphoid hyperplasia.
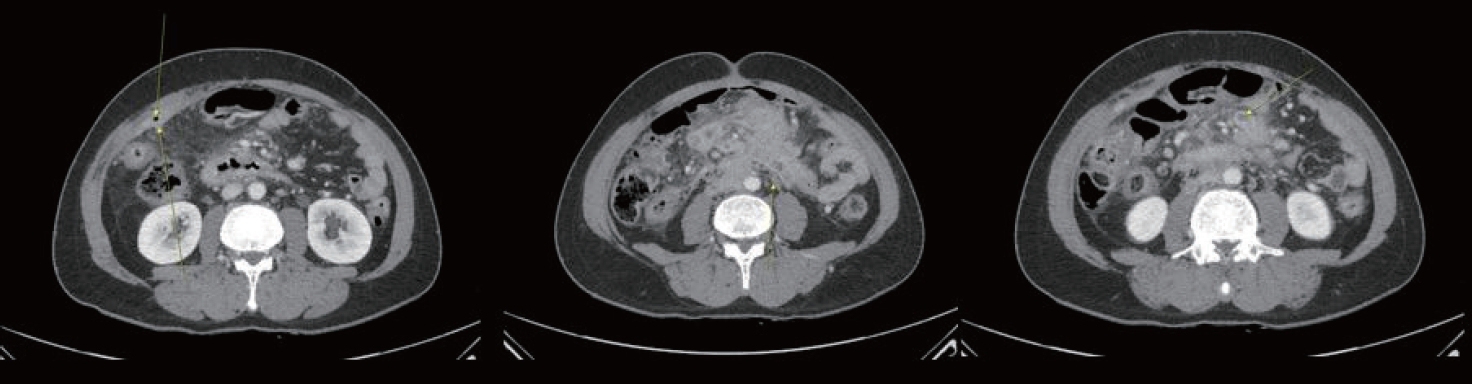
Computed tomography (CT) of the abdomen (Fig. 3), performed at another hospital, revealed a subepithelial masslike lesion in the duodenal bulb and mildly enhanced wall thickening in the proximal duodenum. Mass-like lesions accompanied by severe omentomesenteric infiltration and lymphadenopathy were observed in the right upper quadrant (RUQ) omentum, transverse mesocolon, gastrocolic ligament, and along the ileocolic mesentery. Finally, enhanced wall thickening of the ileocecal valve and terminal ileum was confirmed, and focal peritoneal thickening was noted in the RUQ.
At admission to our institute, the following laboratory values were obtained: complete blood count (CBC), which revealed neutrophil-dominant leukocytosis (white blood cell [WBC] count, 13.89 ├Ś 103/╬╝L), an increased total protein content (8.7 g/dL), reversed albumin/globulin ratio (3.6/5.1), and increased C-reactive protein (110.95 mg/L) values. Esophagogastroduodenoscopy (Fig. 4) and colonoscopy (Fig. 5) were performed on day 1 of hospital admission. An erythematous and elevated polypoid mass was identified on the posterior wall of the antrum, and several polypoid lesions were identified in the second portion of the duodenum. A lesion in the duodenal bulb was recognized as a protruding mass-like lesion, which had been identified at a previous hospital. Polypoid lesions were identified in the cecum, ascending colon, and hepatic flexure. Deep biopsy was performed for each lesion.
The patient developed fever (38Ōäā) in the evening after the endoscopy. Upon consultation with an infectious disease specialist, ceftriaxone (2 g) was administered intravenously, and additional evaluation for the possibility of Actinomyces infection was considered.
Biopsies performed at our hospital revealed similar results to those obtained at another hospital. Tuberculosis polymerase chain reaction test result was negative. The patient reported that he was employed at a recycling center where he mainly worked barefoot on dirty floors. Upon further consultation with the Infectious Disease Department, we determined that the most accurate procedure for confirmation of his current condition was excisional biopsy.
We requested a surgical biopsy from the General Surgery Department. Omentectomy was performed as it was much easier to approach than the other lesions, and we were reluctant to partially resect the patientŌĆÖs colon; therefore, we estimated that omentectomy would be sufficient for biopsy confirmation (Fig. 6). After excisional biopsy, the patientŌĆÖs symptoms improved rapidly despite receiving only conservative treatment. On postoperative day 3, the patient desired to return home. Thus, we decided to interpret the biopsy results at the outpatient clinic and discharged the patient.
Seven days after biopsy, all slides and test results were confirmed. The CBC results revealed a hemoglobin value of 11.4 (g/dL), WBC count of 9.43 ├Ś 103/╬╝L, neutrophil count of 65.7%, and platelet count of 579 ├Ś 103/╬╝L. His lactate dehydrogenase level was 399 IU/L. Tuberculosis-specific antigen-induced interferon-gamma test results were negative. IgG subclass tests revealed an IgG concentration of 2,131 mg/dL and an IgG4 level of 118 mg/dL. The fat tissue was visible in the low-magnification image of the omental biopsy slide (Fig. 7). Moreover, interstitial fibrosis, which should have been absent, was also observed. In the medium-magnification image (Fig. 8), thick septal fibrosis was confirmed, and clusters of lymphocytes or inflammatory cells were observed. Storiform fibrosis, which appeared as bending, was confirmed on a high-magnification slide. Obliterate phlebitis was confirmed (Fig. 9). No red blood cells were detected. A typical cart-wheel appearance of fibrosis was observed [5]. However, the diagnosis of the disease was difficult, because the biopsy results were unclear. On the histochemically stained slide presented in Figure 10, the faintly visible yellowish area reflected IgG, whereas IgG4 deposition was focally confirmed in only one area. Black staining indicates plasma cells. More than 10 IgG4-positive plasma cells were confirmed in a high-power field (147/HPF in a hot spot), and the IgG4-positive to IgG-positive ratio exceeded 50% [6]. Additionally, characteristic diffuse/localized swellings or masses were confirmed in several organs during clinical examination. Consequently, the diagnosis of IgG4-RD originating in the gastrointestinal tract was confirmed.
Three months later, the patient returned to our outpatient clinic with a complaint of abdominal pain, was readmitted, and underwent abdominal CT (Fig. 11), which revealed that the extent of the infiltrative enhancing mass-like lesion had reduced compared with the findings on the previous CT. However, the extent of the infiltrative mass-like lesions visible along the mesenteric root, inferior vena cava, aorta, and small bowel mesentery increased. The patient showed signs of worsening, and first-line therapy for IgG4-RD, that is, steroids, was administered.
After administration of prednisolone (0.8 mg/kg), the patient showed improvement in symptoms and was discharged after one week of hospitalization. At the last outpatient visit, the prednisolone dose was reduced to 30 mg, his abdominal pain had completely improved, and he experienced no problems while performing routine activities. The patientŌĆÖs IgG4 levels also decreased (Fig. 12).
Herein, we present the case of a patient with abdominal pain and multiple tumor lesions in the gastrointestinal tract. Although confirmation was not possible using an endoscopic biopsy, IgG4-RDs were confirmed using a surgical biopsy.
IgG4-RD was identified as a specific type of pancreatitis in an initial case report of a patient with immune-related cholangitis and Mikulicz disease. Later studies established a hereditary form of multifocal fibrosclerosis that progressed to sclerosing pancreatitis and classified it as an IgG4-related sclerosing disease [7].
The exact trigger for IgG4-RD is unclear; however, endogenous antigens and unknown immune responses to microorganisms or allergens are suspected of contributing to the disease. Fibrotic lesions are likely caused by the interactions between activated B cells, CD4+ cytotoxic T lymphocytes (CTLs), M2 macrophages, and fibroblasts. CD4+ CTLs may stimulate cytokine production, promote B cell switching to IgG4, and expand the number of IgG4-positive plasma cells. Fibroblasts secrete extracellular matrix proteins that fill the space created by cell loss following apoptosis. Cell proliferation and extracellular fibrosis lead to the formation of tumorlike masses and organ enlargement. Histological studies have revealed changes such as lymphoplasmacytic infiltration and storiform fibrosis [8].
However, evidence regarding the incidence and prevalence of IgG4-RD remains limited. However, the most credible statistics originate from Japan, which indicates that the prevalence of IgG4-RD is approximately one in every 100,000 individuals [9]. Epidemiological studies of IgG4-RD face key challenges. Many studies were conducted before the disease was widely recognized, leaving many physicians unaware of its diagnosis. Additionally, confirming the diagnosis remains difficult, even for expert practitioners [7].
Patients with IgG4-RD involving the intestinal tract usually complain of abdominal discomfort or pain and may also report symptoms such as nausea, vomiting, and changes in bowel habits. Symptoms suggestive of infection such as fever and chills may also be present. However, the symptoms in patients with IgG4-RD are not uniform and may appear nonspecific.
In patients with IgG4-related diseases involving the stomach, infiltration of IgG4-positive plasma cells has been observed in the gastric mucosa. In addition, gastric ulcers or multiple sporadic polyps with erosions and erythematous surfaces were also observed. Swollen major papillae have also been reported in patients with duodenal IgG4 infiltration [10]. In lesions related to IgG4 in the colon, most biopsied polyps contained IgG4-positive plasma cells. Furthermore, the discovered polyps developed into polyposis involving numerous IgG4-positive plasma cells [10]. IgG4-related pseudotumors have been reported in several organs, including the liver and lungs [11-13].
IgG4-RD is defined by specific histopathological features in various tissues throughout the body. These features differ among different organ tissues. While histopathological findings are often strongly indicative of IgG4-RD, a definitive diagnosis usually requires clinical, laboratory, and radiological evaluations [14]. Evidence-based guidelines for IgG4-RD of the digestive tract were published in 2020 and are summarized below [15].
First, clinical studies reveal characteristic diffuse or localized swelling or masses in single or multiple organs. Second, hematological studies reveal elevated serum levels of IgG4 (Ōēź 135 mg/dL). Third, histopathological studies revealed the following two findings: 1) marked lymphocytic and plasmocytic infiltration and fibrosis, and 2) IgG4-positive plasma cell infiltration with a ratio of IgG4-p4ositive to IgG-positive cells of > 40% and > 10 IgG4-positive plasma cells per high-power field.
If all three criteria were fulfilled, the diagnosis of IgG4-RD was confirmed. If criteria 1 and 3 are fulfilled, the diagnosis is probable. If criteria 1 and 2 are fulfilled, the diagnosis is considered possible.
The initial diagnosis in this patient was difficult for several reasons. First, as cases of IgG4-RD originating from the gastrointestinal tract are less commonly reported than those originating from other organs, tests were conducted to prioritize other diseases [16]. Second, the biopsy posed some difficulties, as biopsies, including the deep biopsy, all revealed chronic inflammation, lymphoid aggregates, and lymphoid hyperplasia. Although many samples were obtained, obtaining meaningful histological results was challenging. In addition, although an excisional biopsy was performed using surgery, confirming the diagnosis remained difficult, as clear evidence for a diagnosis was not found in the tissue obtained; however, it was observed in a localized area. Endoscopic ultrasound-guided fine-needle aspiration should be considered before performing surgical biopsy. Third, symptoms were ambiguous. The patient complained of fever, vague abdominal pain, and discomfort; he did not complain of any additional symptoms, such as nausea, vomiting, constipation, or diarrhea. No weight loss or changes in eating habits were observed. Fourth, it is difficult to definitively rule out infectious diseases. The patientŌĆÖs living environment and socioeconomic status make them vulnerable to infectious diseases. In cases of Actinomyces infection, secondary mass-like lesions accompanied by fever, which is a complicated diagnosis, have been reported.
This case indicates that in patients suspected of having IgG4-RD with the primary site in the gastrointestinal tract, surgical biopsy rather than endoscopic biopsy may be used to rapidly diagnose the patient. In addition, when a surgical biopsy is performed, obtaining multiple samples may help confirm the histological results. Additionally, obtaining a sample using target tissue resection should be considered when planning surgical biopsy.
Glucocorticoids, specifically methylprednisolone, are the first-line of treatment for all patients with active IgG4-RD. Patients with IgG4-RD typically respond to glucocorticoids within a few days of diagnosis [7]. However, the patientŌĆÖs symptoms may fluctuate. Unlike this case, the increase in IgG4 levels may not be prominent [17]. In our case, the patientŌĆÖs abdominal pain suddenly resolved, and the inflammatory reaction was probably suppressed by the antibiotics and various anti-inflammatory drugs, such as acetaminophen, used in his initial treatment. However, the reason for this remains unclear. We plan to conduct further research on this topic. Considering the above, CT or endoscopic examination should be used to determine the initiation of steroid administration rather than symptomatic treatment. Steroid administration should be initiated after observing the worsening of lesion patterns.
Notes
AUTHOR CONTRIBUTIONS
Eun Sun Kim conceived and proposed this clinical case. Young Cheon Ra searched and reviewed reference papers and wrote the case report. Hoon Jai Chun, Yoon Tae Jeen, Bora Keum, Hyuk Soon Choi, Han Jo Jeon, Sang Hyun Kim, and Bomee Lee reviewed draft of the case report and provided advice on the final manuscript.
REFERENCES
1. Stone JH. IgG4-related disease. In: Loscalzo J, Fauci A, Kasper D, Hauser S, Longo D, Jameson JL, eds. Harrison's principles of internal medicine. 21st ed. New York: McGraw-Hill Education, 2022:2837ŌĆō2838.
2. Hirano T, Kawakami Y, Nakabayashi S, et al. A case of immunoglobulin G4-related gastrointestinal disease diagnosed from persistent diarrhea and abdominal pain. Gastro Hep Adv 2023;2:1089ŌĆō1092.



3. Zhang X, Jin X, Guan L, Lin X, Li X, Li Y. IgG4-related disease with gastrointestinal involvement: case reports and literature review. Front Immunol 2022;13:816830.



4. Seo HS, Jung YJ, Park CH, Song KY, Jung ES. IgG4-related disease in the stomach which was confused with gastrointestinal stromal tumor (GIST): two case reports and review of the literature. J Gastric Cancer 2018;18:99ŌĆō107.



5. Deshpande V, Gupta R, Sainani N, et al. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol 2011;35:26ŌĆō35.

6. Strehl JD, Hartmann A, Agaimy A. Numerous IgG4-positive plasma cells are ubiquitous in diverse localised non-specific chronic inflammatory conditions and need to be distinguished from IgG4-related systemic disorders. J Clin Pathol 2011;64:237ŌĆō243.


7. L├Čhr JM, Vujasinovic M, Rosendahl J, Stone JH, Beuers U. IgG4-related diseases of the digestive tract. Nat Rev Gastroenterol Hepatol 2022;19:185ŌĆō197.


8. Umehara H, Okazaki K, Nakamura T, et al. Current approach to the diagnosis of IgG4-related disease - combination of comprehensive diagnostic and organ-specific criteria. Mod Rheumatol 2017;27:381ŌĆō391.


9. Uchida K, Masamune A, Shimosegawa T, Okazaki K. Prevalence of IgG4-related disease in Japan based on nationwide survey in 2009. Int J Rheumatol 2012;2012:358371.



10. Koizumi S, Kamisawa T, Kuruma S, et al. Immunoglobulin G4-related gastrointestinal diseases, are they immunoglobulin G4-related diseases? World J Gastroenterol 2013;19:5769ŌĆō5774.



11. Zen Y, Harada K, Sasaki M, et al. IgG4-related sclerosing cholangitis with and without hepatic inflammatory pseudotumor, and sclerosing pancreatitis-associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis? Am J Surg Pathol 2004;28:1193ŌĆō1203.

12. Zen Y, Kitagawa S, Minato H, et al. IgG4-positive plasma cells in inflammatory pseudotumor (plasma cell granuloma) of the lung. Hum Pathol 2005;36:710ŌĆō717.


13. Tsuboi H, Inokuma S, Setoguchi K, et al. Inflammatory pseudotumors in multiple organs associated with elevated serum IgG4 level: recovery by only a small replacement dose of steroid. Intern Med 2008;47:1139ŌĆō1142.


14. Padniewski JJ, Thottam E, Nasr R. IgG4 sclerosing disease of the esophagus: a case-based review. Rheumatol Int 2020;40:1733ŌĆō1737.


A 2-cm protruding mass-like lesion in the duodenal bulb identified during an esophagoduodenogastroscopy performed at another hospital.
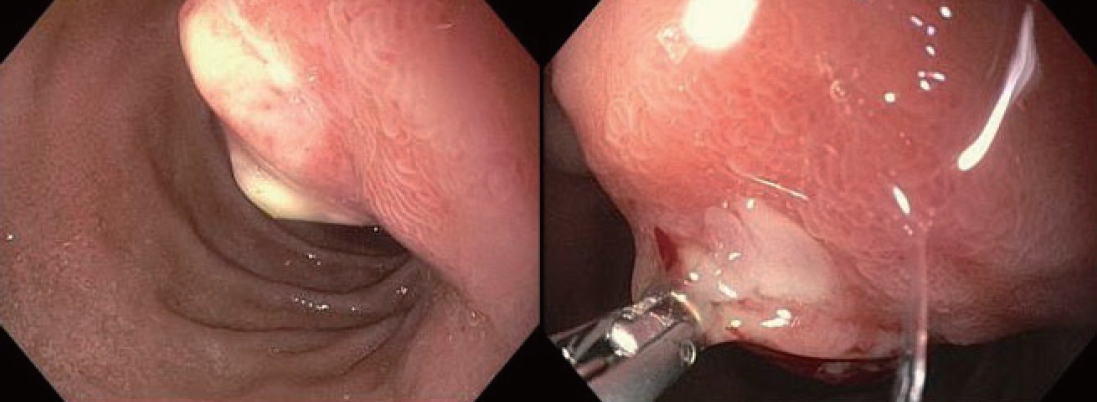
Figure┬Ā1.
Non-contiguous polypoid lesions in the ascending and transverse colon identified during an colonoscopy performed at another hospital.

Figure┬Ā2.
Abdominal CT performed at another hospital showing mass-like lesions accompanied by severe omentomesenteric infiltration and lymphadenopathy were observed in the right upper quadrant (RUQ) omentum (first picture's yellow arrows), transverse mesocolon, gastrocolic ligament, and along the ileocolic mesentery (second picture's yellow arrow). Enhanced wall thickening of the ileocecal valve and terminal ileum (third picture's yellow arrow). CT, computed tomography.
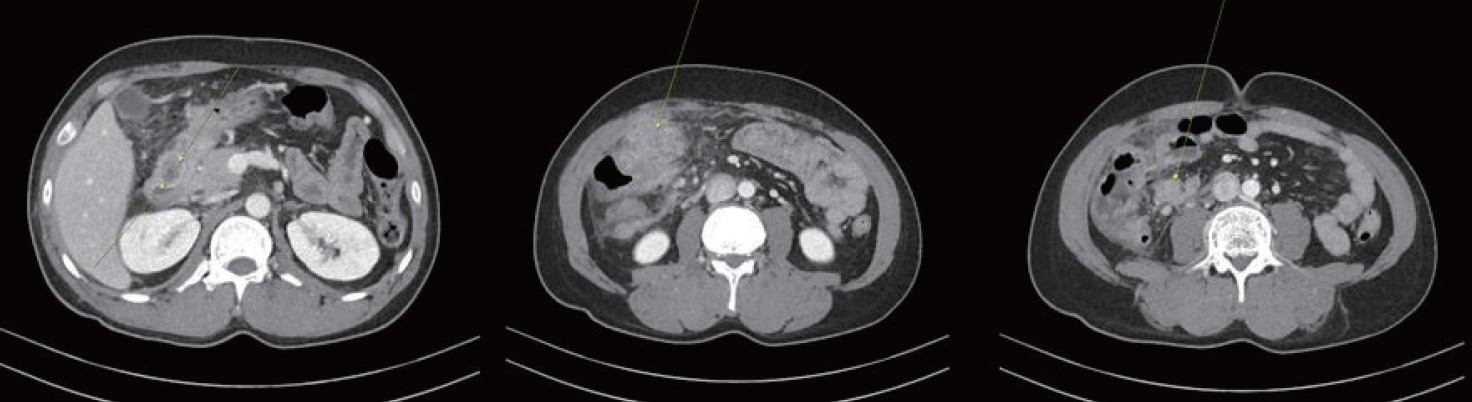
Figure┬Ā3.
An erythematous and elevated polypoid mass was identified on the posterior wall of the antrum, and several polypoid lesions were identified in the second portion of the duodenum during an esophagoduodenogastroscopy performed at our institute.
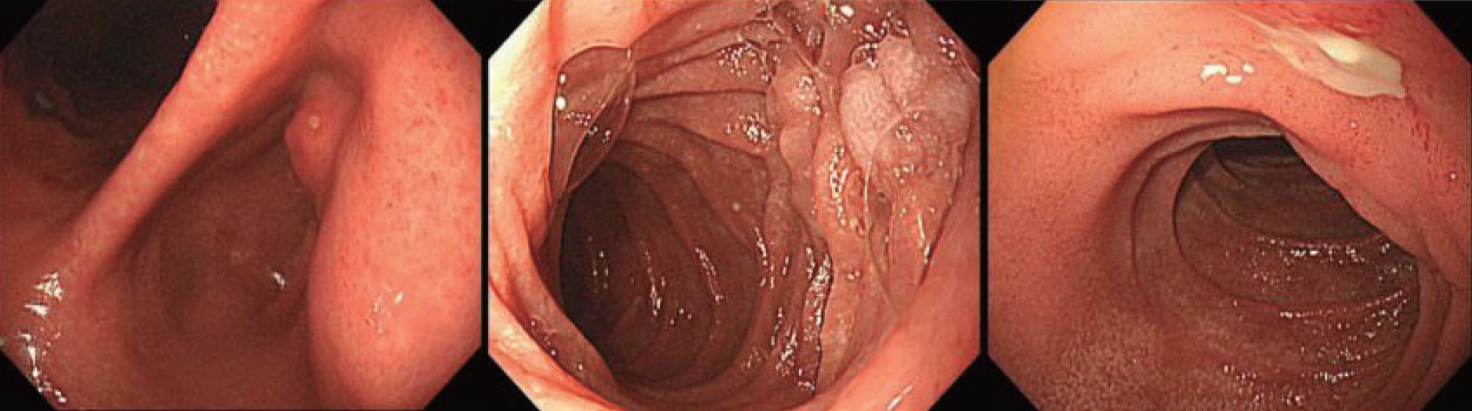
Figure┬Ā4.
Polypoid lesions were identified in the cecum, ascending colon, and hepatic flexure during a colonoscopy performed at our institute.
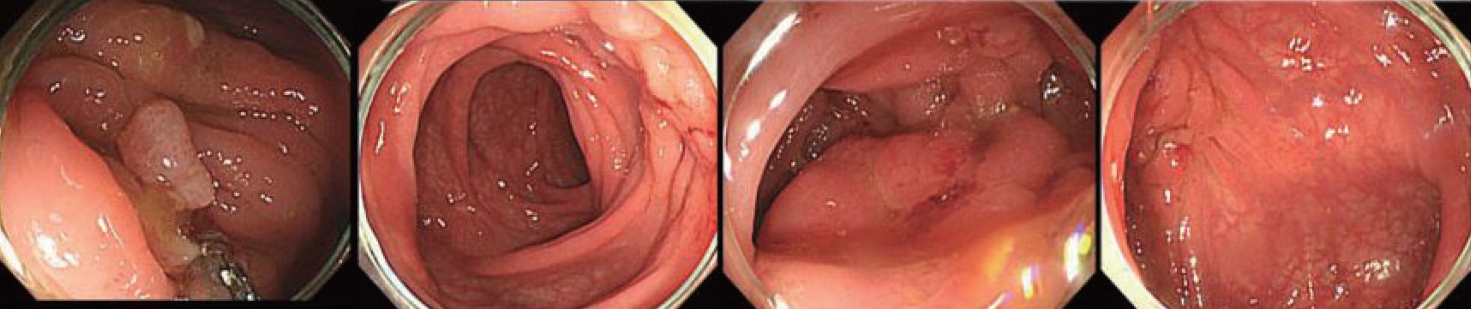
Figure┬Ā5.
The fat tissue and interspersed fibrosis is was visible in the low-magnification image of the omental biopsy slide. ├Ś 100, H&E staining. H&E, hematoxylin and eosin.
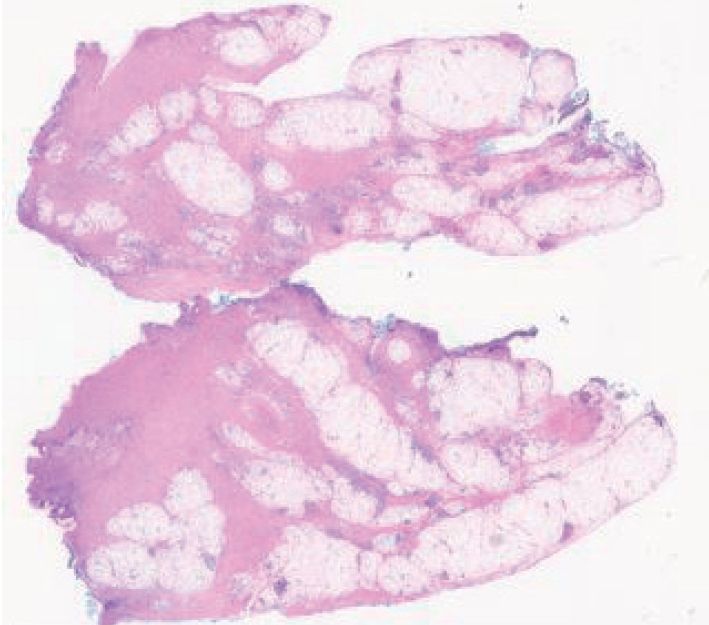
Figure┬Ā7.
Thick septal fibrosis and clusters of lymphocytes or inflammatory cells were observed. ├Ś 200, H&E staining. H&E, hematoxylin and eosin.

Figure┬Ā8.
Storiform fibrosis, which appeared as bending, and obliterate phlebitis were observed. A typical cart-wheel appearance of fibrosis was also observed. ├Ś 400, H&E staining. H&E, hematoxylin and eosin.

Figure┬Ā9.
The faintly visible yellowish area reflected IgG, whereas IgG4 deposition was focally confirmed. Black staining indicates plasma cells. ├Ś 400, IgG4 immunohistochemical staining. IgG, immunoglobulin G.

Figure┬Ā10.
Mass-like lesions accompanied by severe omentomesenteric infiltration and lymphadenopathy were observed in the right upper quadrant (RUQ) omentum (first picture's yellow arrows), transverse mesocolon, gastrocolic ligament, and along the ileocolic mesentery (second picture's yellow arrow). Enhanced wall thickening of the ileocecal valve and terminal ileum (third picture's yellow arrow).



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




